Scientists make this season's flu vaccine based on the strains of the virus that circulated during the last flu season. It's a flawed approach, but it's the best they can do given that it takes months to make the vaccine, and there's no way -- at least not yet -- to predict how the virus might evolve in the interim. But a new computer modeling study suggests the human immune system has a better memory than scientists had thought for strains of the flu it's encountered in the past. In the future, the researchers say, it might be possible to exploit this to design better vaccines.
Every year, the flu wreaks havoc around the world. It typically infects millions of people around the world every year and kills up to 500,000 in a typical year. National economies lose billions of dollars to medical care and missed workdays.
The flu vaccine helps soften the blow, but vaccine makers are in an arms race with the virus. The Global Influenza Surveillance Network (orchestrated by the World Health Organization) continuously collects samples from ill people all over the globe and in February each year chooses which strains to put in the vaccine. Months later, around November, people start rolling up their sleeves to receive a vaccine based on those one or two strains. But sometimes the virus mutates during the lag time between spring and fall, which renders the vaccine less effective.
"If the virus has evolved, the vaccine's efficacy is not as good as it could be," explains virologist Derek Smith from the University of Cambridge, "But it's still better to be vaccinated than not at all."
Smith thinks we can improve the vaccine, even if we can't accurately predict the flu's evolution yet. His new study published in Science today offers a new way to look at our immune system's reaction to influenza. The team tracked 64 people in Vietnam for six years, analyzing their antibodies -- proteins made by the immune system to flag invading pathogens for destruction -- when they were infected with the flu.
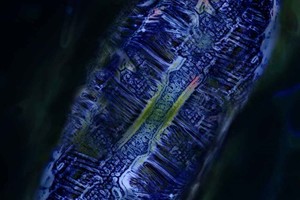
They then created 3-D "antibody landscape" maps of each person's immune response, says research assistant and co-author Sam Wilks. In the figure above, the colored dots represent different strains of flu, and the space between the dots reflect structural differences between those viruses. The 3-D landscape (blue) shows the individual's varied immune response to all the strains (peaks indicate high immunity, valleys indicate low immunity).
The landscapes revealed something remarkable: when influenza infects someone, it not only triggers an immune response for that particular strain, but for all the strains of that type of flu that have ever infected the person. This phenomenon, named 'back-boosting,' means that our old immunity gets boosted every time we're faced with a new flu virus. Typically, the back boost response was stronger for past strains that were closely related to the infecting strain.
The researchers think we make antibodies for past strains because our immune system's memories of past viruses are activated more easily than they'd thought. The findings suggest that the flu vaccine provides much more protection than anyone thought against past versions of the flu that have infected a person. Someone infected with the flu last year will still make antibodies for that strain, regardless of what version of the vaccine they receive. "It's essentially a free pass," Smith said.
This means scientists can try to predict how the virus might mutate (an active area of research) and base a vaccine on that, without worrying about diminishing protection against current circulating strains. If last year's strain is still around this flu season, a vaccine targeted for a novel strain will still offer a defense by stirring antibody production. "This opens up the possibility for vaccinating against a future virus," explains Smith, "We don't have anything to lose because it won't make the vaccine any worse. The back boost covers our backs."
Epidemiologist Michael Osterholm agrees. "This is potentially revolutionary work," says Osterholm, who directs the Center for Infectious Disease and Research Policy at the University of Minnesota, "We're a long way from changing our current policies, but this could really help. It also raises questions about how often do we need to be vaccinated if we can use this back-boost?"
It'll be a while before a vaccine that takes advantage of the back-boost goes into a shot or nasal spray -- the approach still needs to go through clinical trials, which Smith hopes to get started on within a couple years. Until then, he recommends you get your flu shot anyway.

An “antibody landscape” map showing one person’s immune response to different strains of influenza (see text for more explanation)
Center for Pathogen Evolution, University of Cambridge
